“When there’s successes, I credit the team… when there’s failures, I own it, it’s on me. That’s the leadership style because I need my team to feel positive. It’s not an ‘I’, it’s the team. I’m always using we in my communication: ‘we, we, we’. All the way home!”
April 2020
In this session of Quality Time: Sharing PIE, Cindy Gilman from Carrol County Memorial Hospital in Carrolton Missouri, and Karen Hooker from Kit Carson County Health Service District in Burlington Colorado, healthcare professionals from very different backgrounds, talk about how they became quality leaders.
Want to take Quality Time with you on the go? You can subscribe to the podcast version through your favorite streaming service.
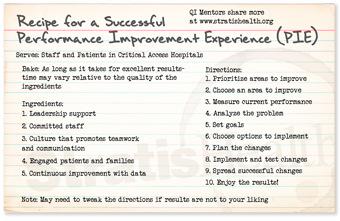
Insights from your QI Mentors
Recommended resources
 Select resources recommended by the QI Mentor Program.
Select resources recommended by the QI Mentor Program.
- NAHQ/CPHQ Certification. The National Association for Healthcare Quality (NAHQ) Certified Professional in Healthcare Quality (CPHQ) is the industry standard certification for the healthcare quality profession.
- Lean Six Sigma. Lean Six Sigma is a fact-based, data-driven philosophy of improvement that values defect prevention over defect detection. It drives customer satisfaction and bottom-line results by reducing variation, waste, and cycle time while promoting the use of work standardization and flow, thereby creating a competitive advantage. It applies anywhere variation and waste exist, and every employee should be involved.
- Stratis Health QI Basics Course. This online course is designed to equip professionals with the knowledge and tools to start quality improvement projects at their facilities. Online courses may be completed in sequence, or individual modules and tools may be used for stand-alone training and review.
 Second helping of PIE?
Second helping of PIE?
If you would like more information from the national virtual Quality Improvement Mentors on their performance improvement experience in critical access hospitals, please submit this short form.
| QI Mentor favorite featured pie recipe: Pioneer Woman’s Pecan Pie |
 |
Transcript: Becoming a QI leader
Note: Quality Time: Sharing PIE is produced for the ear and designed to be heard. This transcript is intended to augment the recording.
Narrator: Welcome to Quality Time: Sharing PIE, when experienced quality improvement staff from critical access hospitals across the country sit down together and serve up their lessons learned—strategies, tips, and ideas—from their in-the-field performance improvement experience.
Sarah: Hi – I’m Sarah Brinkman from Stratis Health. Thank you for listening to this session of Quality Time: Sharing PIE. I’m excited to be joined today by Cindy Gilman from Carrol County Memorial Hospital in Carrolton Missouri and Karen Hooker from Kit Carson County Health Service District in Burlington Colorado! So glad you two Quality Improvement Mentors can sit down with me today to talk about how you became quality leaders.
Sarah: You two came to quality with very different backgrounds. Karen, you started as a respiratory therapy aide and became a nurse after you transitioned into quality. And, Cindy, you started as a nurse in long-term care where you picked up quality then moved into the hospital setting. So, I’m curious, what launched you into quality? Why were you tapped to be a quality improvement leader?
Karen: I always said yes. When something came up and the CEO asked me to do something or my boss asked me to do something, I said, “Yeah, sure. I’ll do it.” I may not have been qualified to do it. I may not have the full knowledge to do it, but I always said yes… we had a CMS survey that didn’t go so well, and they needed someone to run the infection control program. And so, they asked me, and I said yes… I shared the office with an EMS director and when she resigned, they asked me if I wanted to take over just because I shared the office with her and I said, “Well sure, yes.” Then the quality position needed a leader. The CEO said, “Would you like to do quality?” And I said yes.
Cindy: I always try to lead the group. I’ve always been that way, even in school. I always spoke out and gave my opinion whether it was right or wrong, and I feel like you need to do that. You can’t be quiet, especially with quality. And I think that’s a big thing. You can’t be quiet. You got to be loud and proud. Karen, she mentioned being a yes person, but to be a yes person, you’ve got to be that person willing to do the research, find your resources, gather the information. And I think that that is a big thing with being that yes person.
Sarah: “We know that all successful quality improvement professionals include themselves in the improvement process, so we wanted to know what Karen and Cindy did to further their quality work when they first got started.”
Cindy: I had to learn everything and so I jumped right in, learned what I could. If I didn’t know the answer, I reached out and tried to get that answer… got myself involved with Missouri Hospital Association as much as I could, and I really feel like that’s what helped me along my way.
Cindy: And I think not being afraid as well, I’m emailing other hospitals, I’m reaching out to other people. What are you doing? What’s best practice? What do we need to do? Do we need to do something different? And I think you always have to keep doing that. You can’t stop. You always got to keep reaching out to others and seeing what everyone else is doing and seeing if there’s anything else you can do different.
Karen: I had such a great network in Kansas, and I moved to Colorado and then it was like a desert: dry. And the Colorado Hospital Association put on an infection control, or infection prevention program in our community and area hospitals came to my community. And I’m like, “You ladies aren’t leaving until we exchange emails and we connect with each other because I’m dying here. I need those resources.”
Sarah: We asked Karen and Cindy to share some of the barriers they faced during their QI career journeys, and what lessons they learned from them.
Karen: My very first quality improvement activity I did was a flop, absolutely a flop. I had way too many people involved. We didn’t do any small testing to make sure it was going to work. Frontline staff probably wasn’t involved in the way they should have been. Rolled it out and it failed miserably, and we never got that project back off the ground because it was such a colossal failure. So, for me, the roadblocks were the lack of knowledge, the lack of quality tools I needed to make improvement. But again, I learned from my mistakes and then moved on and then got the resources I need.
Cindy: Sepsis was a new core measure, and that was my first project here and I learned a lot from that, probably one of the big things was I invited way too many people to that meeting. It was overkill and then I didn’t have a duty for each person that was on that committee. So, I learned that lesson…
Karen: I confess, I had no shame saying, “I failed here, I did this wrong. I failed; this is what I should have done. Let’s move on.” So, I owned it.
Sarah: “Our mentors went on to describe the importance that accountability, teamwork, and recognition play in successful quality improvement.”
Karen: When there’s successes, I credit the team. The team gets all the credit for the successes. When there’s failures, I accept the failures. I own it, it’s on me. So that’s how I build my team up. And that’s the leadership style because I need my team to feel positive. …It’s not an I, it is the team. I am always using we in my communication that “we, we, we”. All the way home.
Cindy: Quality is definitely a team effort. It’s not one person …the big thing is just … Thanking someone also goes a long way. They may not necessarily want a pizza party but just to be recognized and appreciated I think is huge and important.
Sarah: You’ve both been in your role now for a while. … What do you wish you knew when you took on your role in leading quality or what are the key skills you’ve picked up along the way that you would encourage others to seek out?
Cindy: Tim Braun, he is our COO, and Tim came to us with his Lean Six Sigma Green Belt, and he was showing all these different things that he had done with his Lean Six project. And I was like, “Oh my goodness, this is very interesting. I think this is something I need to do.” And it just so happened, Missouri Hospital Association sent out an email offering Lean Six Sigma classes. And so, I was accepted into that and I was able to participate in that and obtain my Green Belt.
Karen: What I wish I would have known was to …. Get into a class to learn about the quality tools, reach out to my peers and people that could help me with it. And something that I did recently is I went through the Certified Professional Healthcare Quality certification and the stuff I learned in that program was amazing.
Sarah: So it sounds like training has been important to inform how you approach quality. What tools or resources have you found to be most useful in your work?
Karen: Healthcare people are very scientific and so they want to see the proof and when you have that- those charts that they can actually visualize what’s going on with the data. They have a better buy-in with that. So, I use my run charts and control charts.
Sarah: Cindy, I know you’ve mentioned before using quality boards. Can you talk a little bit about the intent behind that…?
Cindy: The intended audience for that is the staff in that department, so I want the staff to be able to go to that board and say, “Hey, this is where we’re at with our turnaround time.” Look at the project, and “this is where we want to be at and the interventions to get us there.” We use green, yellow, and red. So, I think the color coding is important. It’s a quick at-a-glance for staff and they say, “Oh my goodness, that’s in red. That’s something we really need to work on.”
Sarah: What do you understand about your role now that you wish you knew when you were starting out in quality? When you were younger and more naive?
Cindy: I’d say with me that it’s not all my responsibility. I felt like it was, but in the end, again, those department directors, they have to be involved in the process. They have to take ownership and accountability for the quality that their department is producing, and I think that’s huge. If I’d have known that in the beginning, I would’ve done things a lot differently.
Karen: That’s exciting to hear, Cindy, because so many times in the smaller facilities, frontline staff and department leaders believe that the quality is owned by that quality person
Cindy: And a lot of them are working managers, working directors, so quality was kind of put on the back burner essentially. It’s almost like checking a box, you know? And I feel like now they understand the importance of it. And they know when they come to the quality meeting, if something’s not where it needs to be, I’m going to question them. They know that, but they also know that they can come to me and I will help them through the process. The leaders are now coming to the quality meetings and participating. And that’s big because when the directors see those leaders there, they’re thinking, “Oh my goodness, I got to get my stuff together. I got to be prepared to answer to them why my quality is not where it needs to be.”
Sarah: Recognizing that good leaders surround themselves with good people, we wanted to know how our quality improvement mentors surround themselves or build up others to support their leadership.
Cindy: Well, it’s going to shock everyone, but I don’t really care for data. I’m not good with Excel. I know the bare minimum, so I have multiple people within the organization that I can go to. I’ve got report builders that I can reach out to. I’ve got my COO who loves data …
Sarah: Identifying opportunities and implementing quality projects are obviously a big part of your work – how do you work with your teams to sustain improvement over time?
Cindy: I think a big thing that I really didn’t talk about, and that’s the pulse check, going back, and that’s one thing that I really need to work on as a quality leader is just going back. Once you complete a project you can’t just forget about it. And I think that’s really important and that’s very easy to do. And so, as quality leaders, we need to go back, and check and you can’t always run a report to check that. You might need to go out and actually watch it in action to make sure that it’s still working correctly.
Karen: Workarounds are huge in hospitals and we all have our workarounds and so we can get rid of them by going back and checking and making sure that we actually have a process that doesn’t require workarounds.
Sarah: We ended our sharing PIE conversation by asking our mentors what keeps them pumped up to do this work on days when maybe things aren’t going so great or something doesn’t go quite the way they want.
Karen: For me is if it’s a personal thing, every day is a new day… I don’t let things steal my joy. I may be sad for a moment, but, I quickly, I’m grateful for the other things and so my joy is not stolen.
Cindy: I’m fortunate that I have a walking track right across the hall from my office. So maybe I need to go for a walk, listen to some Post Malone, so I’ll do that. … I’ve always been one, I just make it work; I just deal with it and make it work and go on.
Narrator: Quality Time: Sharing PIE was produced by Stratis Health, with funding through Rural Quality Improvement Technical Assistance, a program supported by the Federal Office of Rural Health Policy, to help critical access hospitals across the country move from quality reporting to quality improvement. Want another serving of PIE? Or have a burning question about rural quality improvement? Visit the QI mentors web page.


