“We all have to work together as a team to make our facility successful and working together in quality is one of those ways that we can be successful.’”
December 2020
In this episode, QI Mentors Cindy Gilman from Carroll County Memorial Hospital in Carrollton Missouri, and Christy Mintah from Avera Holy Family Hospital in Estherville, Iowa discuss how to engage the whole hospital team in quality improvement.
Want to take Quality Time with you on the go? You can subscribe to the podcast version through your favorite streaming service.
Insights from your QI Mentors
Recommended resources
Select resources recommended by the QI Mentor Program.
- Sample template for department presentations to a quality committee.
- Sample QI department report template.
- Example – organization-wide QI newsletter.
- Example – “Quality Board“.
Second helping of PIE?
If you would like more information
from the national virtual Quality
Improvement Mentors on their
performance improvement
experience in critical access
hospitals, please submit this
short form.
| QI Mentor favorite featured pie recipe: Apple Crisp Cheesecake Pie |
 |
Transcript: Engaging the Whole Team
Note: Quality Time: Sharing PIE is produced for the ear and designed to be heard. This transcript is intended to augment the recording.
Narrator: In this episode of Sharing PIE, QI Mentors Cindy Gilman from Carroll County Memorial Hospital in Carrollton Missouri, and Christy Mintah from Avera Holy Family Hospital in Estherville, Iowa discuss how to engage the whole hospital team in quality improvement.
Cindy: So, for me, as far as engaging frontline staff and our quality impact teams, I think the huge piece here is it starts at the top. And so in order for the frontline staff to have buy-in and to be engaged, we really need to have leadership, engaged in quality and so for us, having leadership participate in our quality meetings, have, having them visit departments, you know, and dis- discuss quality, with individuals within the department, having the director, you know, speak about quality and having, buy-in as well, encourages the staff to do the same thing. So, I think it’s really important that you know, we start at the top and have leadership engagement.
Christie: Cindy, I totally agree with that, also one other strategy that we utilize here is that when our directors are talking to our frontline staff, we get our ideas from some of the frontline staff. we go to them and we have open conversations with them and say, what’s working, what’s not working for you. And then we help them, to develop performance improvement and quality projects, based off their ideas of what’s not working so well for them in their daily routines.
Cindy: I think that’s a great point, Christie. you do have to go to the frontline staff and find out, you know, what isn’t working for them because they are the ones out there doing the work, day in and day out, and they see what works and what doesn’t.
Cindy: One thing that was brought to our attention was our workflow in our outpatient specialty clinic. And there seemed to be a delay. so patients maybe had a delay in seeing the physician they had scheduled an appointment with. And so we really took a hard look at the processes and workflow in that clinic. And, you know, what we found was that a lot of our patients, after they would check in and for the outpatient clinic, they would need lab work or they would need radiology. So then they would have to go to the other end of the hospital to have, radiology completed, to have lab work completed. And what we found was that just really did not work for the clinic and for the patients. We noticed our patient satisfaction scores were going down and it just was not a good workflow. And so we took a hard look at that. we put a group together and looked at the process and the workflow, we did some time studies from the point of check-in to check-out to see you know, what was going on. And so from that, we were able to, identify that, you know, we could, for example, in our urology clinic, complete the UA, in the outpatient clinic, therefore the patient did not have to go back to the lab to get that completed. And so by doing so we were able to reduce our, our times for patient waits in our outpatient clinic and then, therefore, improve patient satisfaction.
Christie: Cindy, that’s a great example. We also look at workflow situations. Our staff helped us to meet the CMS measure for stroke patients coming into the ED. They’re supposed to have their CT scan within 45 minutes of arrival. And it was our paramedics who work in our ED part-time that came to us and said, “Hey, why are we stopping in the ED when radiology is clearly at the other end of the building? Why aren’t we pulling up to the back door the closest to radiology, stopping, getting the CT scan and then heading down to the ER?”And so we implemented that and that improved our scores in that measure significantly.
Narration We asked the Mentors to talk a little about process and communication strategies
Christie: I found from my own personal experience that the more formalized the process is and the more organized the process is, the more that you can see it and measure it and know that something’s being done. The more informal that you leave the process, the more gray areas that you see, and it’s harder to measure or even account for better outcomes.
Cindy: And Christie is something that we’ve talked about previously is formats and different things that we use. and then oftentimes that in our organizations, we’re doing projects all the time and we’re not writing them down and we’re not taking credit for those. And so I feel like that’s very important that you mentioned the formalized process and that’s something we’re working on really hard here at Carroll County. I think that’s really important having that universal way to show your quality information.
Christie: Yeah. And how are you going to formalize that with what kind of templates, Cindy?
Cindy: We’ve transitioned to a quality board where the department is putting the template. So that’s their quality improvement project that they’re, they’re currently participating in or working on. They’re placing that on the board so that all staff are aware of, you know, what their goal is and what their interventions are. And then they also put on there when it’s completed. So I think it’s really important to have that at the forefront for staff to be able to review.
Christie: Yeah. Can anybody else, besides frontline, frontline staff see that board?
Cindy: yes. If other members of the hospital were to come in, they are welcome to see that, and one department I’m, I’m very proud of is Environmental Services. So trying to come up with a quality goal for them they are on it. And so they have their board and their department.
Christie: That’s interesting to me because sometimes departments like Environmental Services or Plant Operations, they don’t think they have a big role to play in quality. And honestly, they really do. And I also find that once I, I engage them and ask them to do something, they get pretty excited, and they want to do it. And I don’t get the grumbling of… from them about, “Oh, I can’t do that. That’s not part of my role.” They’re usually excited.
Christie: We all have to work together as a team to make our facility successful and working together in quality is one of those ways that we can be successful.
Christie: We’ve all sat in those meetings where it’s all over our head and we don’t have any idea what, what they’re talking about or why it pertains to me. And so, I tend to have a group meeting where all the leaders are together and we talk about quality and the quality goals for the year, but then I go and follow up with having some leaders invite me to their department meetings, and I will go over the quality goals with them, because maybe they don’t feel as comfortable as other leaders in explaining it to the frontline staff and what the quality goals are. So, a lot of the departments post their measures and their outcomes each month. We haven’t gone to a formal process like the communication boards that, Cindy talked about. but I think it’s a great idea, definitely a place where we can go ’cause we can all grow at quality.
Cindy: I completely agree with you, Christie. And I’ve always made it a rule that, if you cannot attend the meeting, I’m not going to review your data because I can’t explain – I want the director to be able to explain what their project is to the group. And so that’s one thing we’ve implemented, because as a quality director, when they are reviewing their information, I would have questions for them and maybe suggestions. And I think that’s something that the whole group can offer to them as well. I think that’s really important to have that open-door policy that they can come in and bounce ideas off of you.
Christie: In order for our senior leadership to be engaged in quality we get together every other week and it’s only for like about a half hour, maybe 45 minutes. And they know what the quality goals are for the year, but we get together, and we look at the data together.
Cindy: I think that’s a really important point. I like that you do get together with them and talk about your goals. And, and I know for us, I mentioned that our quality meetings are monthly, but something we started we are not reporting out every department quarterly, we’re on a rotating schedule. And so that has made a huge difference because our quality meetings would sometimes take over an hour. I do know that when our CEO attends the meetings, you know, the staff know (laughs) he’s going to be asking you questions, you know, you better have s- you better have some answers, you better be able to explain. So I think that’s important too, to, to keep them on their toes and to keep them engaged in the meeting.
Christie: Your idea or your thought on, the pairing down who reports, we’re just starting that process and we are going to go to that limited reporting as well because we also found that long, drawn-out two-hour quality meetings are, are too much.
I’ve developed a prompting question type of form that each person on the committee will get so that you can at least ask a few questions. And it has questions on it. Like what if you compared blank to blank, what would it look like? how does blank affect blank? You know, just to give them prompting questions from the information that they can follow up with when the leader is presenting.
Cindy: Christie, I think that sounds like a great plan. I’m anxious to hear how that goes for you. I think it’s important that you’re asking, members of that committee to ask questions to the person presenting because that does show the person presenting the information that they care and that they’re engaged and they want to know more about it. So oftentimes we feel like we’re doing… or I shouldn’t say myself, but I feel like others think it’s just a check the box. You know, I’m just trying to check this off my list. And that’s, that’s not what quality is about it’s not a check the box.
Narrator: We asked the Mentors to share some obstacles to effective communication they’ve experienced, and how they’ve overcome them.
Christie: I would start by saying that the obstacles to effective communication come from lack of communication about the common goal. some people don’t see the goal and don’t understand the common goal right away.
Cindy: Christie, I think you made some very good points, and I think it’s important also to mention that a lot of times they want to know the “why,” the “why” behind it, “Why are we doing this? You know, why do we have to do this, you know, explain it to me.” And I think that’s really important. You reach a certain point. If you’re showing the same thing, you’ve done the same thing for 10 years, you know, it’s time to present in a different way. It’s time to show something different, whether it’s just the graph that you’re using or, you know, the way that dashboard looks, change it up. you know, try to do something eye-catching. I know something we’re working on here is our patient safety goals with our new quality director. And so I’ve asked her to reach out to marketing, have marketing help you make this pretty, make it eye-catching, make it easy to read.
Christie: Resistance is gonna happen in quality no matter what. And a lot of it has to do with lack of understanding. so you have to be ready for it. But my best advice about resistance is when you have those naysayers, you have to, um… as a quality leader, you have to work with the leaders, you have to… because they’re the ones that are hearing all the negative comments and the, why do I have to do this?
The nursing leader gave me a great example of how to get a naysayer on board. And we had just implemented, Medsafe scanning, and our, we had kind of at the beginning given our EDE kind of that caveat that, “Hey, if you’re super busy, while we’re learning this, you know, take care of the patient, make the patient care first, we’ll, get Medsafe scanning down later.” Well, they took that caveat to the extreme, and we were six, eight months into Medsafe scanning, and their rate was still like in the teens.
So we need to reframe this whole conversation and you know, get them to change. You have to look at your workflow, you have to make this part of your workflow. And so after multiple conversations and coaching on why it’s important to change your workflow to make Medsafe scanning happen we finally are starting to reach our goals. And the leader in that department sends out individual scan rates every month.
And she literally does put the email, “You have the lowest scan rate this month.” “You have the highest standards this month,” because it gives them that competitiveness, everybody responds to competitiveness and nobody wants to be the worst player in the group. And so if they know that, then they respond accordingly.
Cindy: I’m gonna guess that some of those employees have been at your organization for a long, long time. that seems to be the people that are resistant and hesitant to change. It’s, you know, “We’ve always done it this way, why do we have to do it this way?” It’s, you know, “We’ve done it this way for 15 years.” Well, that’s part, part of the reason why we need to do it a different way.
Christie: That’s the one thing with quality and resistance is sometimes you have to answer the question of “what’s in it for me?” And so therefore, you know, you really have to put the “why” behind “what’s in it for me?”
And, and that’s a big deal for some people. So you have to recognize that they’re not going to probably change their habits that they’ve had for 25 years if they don’t know what’s in it for me. And what’s in it for them is making them understand that it’s the best thing for our patients. It’s a way for us to improve the quality of care that we provide to the patients that we serve every day.
Cindy: I think that’s really important, Christie, ’cause that’s why we’re all in healthcare. I mean, that’s why I became a nurse, it’s to provide patient care and to make sure that we’re providing the best care possible.
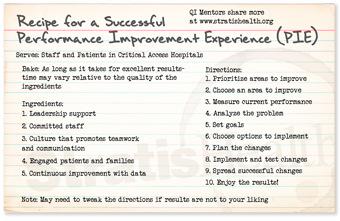
Narrator: Quality Time: Sharing PIE was produced by Stratis Health, with funding through Rural Quality Improvement Technical Assistance — a program supported by the Federal Office of Rural Health Policy — to help critical access hospitals across the country move from quality reporting to quality improvement. Want another serving of PIE? Or have a burning question about rural quality improvement? Visit the QI mentors web page.