“Every time there’s a fall, we have a fall audit that’s done. These audits help us look for trends and opportunities for improvement.”
July 2023
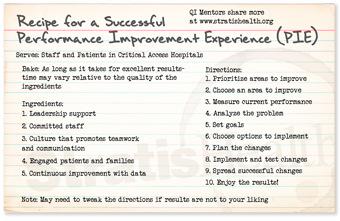
In this session of Quality Time: Sharing PIE, QI Mentors Gloria Barth from Harrison County Hospital, Corydon, Indiana, and Jen Monzo, from McKenzie Health System, Sandusky, Michigan, share how they implemented successful fall prevention strategies at their critical access hospitals.
Resources from this episode
Want to take Quality Time with you on the go? You can subscribe to the podcast version through your favorite streaming service.
 Gloria Barth Gloria BarthHarrison County Hospital Corydon, IN |
 Jenifer Monzo Jenifer MonzoMcKenzie Health System Sandusky, MI |
Transcript: Fall Prevention Strategies
Note: Quality Time: Sharing PIE is produced for the ear and designed to be heard. This transcript is intended to augment the recording.
Narrator: In this session of Quality Time: Sharing PIE, mentors Gloria Barth from Harrison County Hospital in Corydon, Indiana, and Jen Monzo from McKenzie Health System in Sandusky, Michigan, share how they implemented successful fall prevention strategies at their critical access hospitals.
Jen: Hi. My name’s Jennifer Monzo and I’m the Director of Quality and Risk Management at McKinsey Health System in Sandusky, Michigan. I help to ensure that we have effective fall prevention program throughout our hospital.
Gloria: Hi. My name is Gloria Barth and I am the Performance Improvement and Quality Manager here at Harrison County Hospital, in Corydon, Indiana. And as the quality director, one of my responsibilities is monitoring and continuously improving our fall prevention i-… here at the hospital.
Jen: Awesome. So, Gloria, how are you helping to prevent falls in your organization?
Gloria: Well, years ago, we developed a fall prevention team. And it was to educate, reduce the risk of falls, keep lines of communication open daily, all on fall prevention. Because of the pandemic, we were struggling to keep every department communicating with each other. It was like we became silos. So we wanted to change that, so we decided to come up with a project to improve fall prevention as a video. And with that video, we wanted each department we initiated a contest, where every department had the opportunity to come up with a theme song for our fall prevention dance video. And (laughs) this created lots of excitement fun, and communication between departments got so much better. And we weren’t just talking about the pandemic, we were talking about this crazy video that the quality director wanted us to make for fall prevention. But… So it gave everybody something fun to talk about.
Jen: So how did you get your staff on board with this?
Gloria: Well, with the help of our radiology manager, Jamie, we created this contest for everyone to help us pick out this song to promote fall prevention. We put flyers everywhere all over the hospital, the physician offices, EMS. And we told them that, “This is a contest and, and whatever department wins gets a big pizza party.” So they were all for it. So the winning song ended up being Justin Timberlake’s Can’t Stop the Feeling. We then created a dance video and got each department to be a big part of it. Um, they lip-synced and danced to Can’t Stop the Feeling.
Jen: Wow. That sounds like so much fun. Um, I bet that staff really like learning from their coworkers, especially when it’s in an entertaining type format, so that’s pretty awesome. I might have to steal that idea from you.
Gloria: Yeah. Yeah. It was… it was a lotta work, but it was worth it. It took almost a year to put it together.
Jen: Wow.
Gloria: But it… but it was perfect timing because the pandemic caused everyone so much stress. And I noticed by creating this video, it brought so many smiles and positive feedback throughout the whole entire hospital, as well as promoting teamwork again instead of silos.
Jen: Right. I’m sure staff really appreciated the diversion too. Uh, what other things have you implemented with your fall reductions?
Gloria: Well, we have blue blankets that we put on the beds which immediately notifies anyone who comes into the room the nurse, or the nurse’s aide, or the doctor, or the respiratory therapist, anyone that the… if the blue blanket is on the bed, they’re a fall risk. We have falling leave mag-… leaves magnets that we put on the side of the door to let people know as they walk in the room. We have yellow non-skid socks for the patient. We also have a little yellow triangle plastic piece that goes on the ID bracelet that also alerts staff that this patient is a fall risk. We also put up daily postings of how many days that we have not had a fall.
Jen: That sounds like a lot. That’s great. So did you decide on specific goals when you implemented your changes?
Gloria: Well, our main goal was to help staff understand that everyone is responsible for reducing the falls. So our goal was to engage staff with each other, get everyone to be accountable to prevent falls, and to continuously educate and communicate. And most of all, decrease patient falls.
Jen: Right. So how did you share this with your staff?
Gloria: Well, once we got the fall prevention video made, which we thought it turned out pretty hilarious because we got our CEO involved, we got staff from every department, we got doctors involved, nurses. It was… it was such a huge team effort. But the fall prevention video, it’s shown every… at every new employee orientation. And the physical therapist, A- Ashley is a… is the one who shows it. And then she also explains to them all the tools that we use to help prevent falls in the patients’ rooms. It is a hit when they watch the video, seeing staff dancing and lip-syncing to Justin Timberlake’s Can’t Stop the Feeling. And it’s one of the last things they show, so it’s, like, the last thing, you know, when they… when they’re done with orientation, that’s what they remember the most.
Jen: That’s great. I watched your video and it put me in a good mood right away.
Gloria: (laughs) Oh, good.
Jen: (laughs) What made you focus on fall reduction?
Gloria: Well, for this past year, for 2022, ’cause we did all this between 2020 and 2021, especially during the, you know… right in the middle of the pandemic, we needed something to build morale, so that definitely… it was a good choice that we made. But when we did an audit for this past year, 2022, we found a trend. It was the placement of chair alarms they weren’t being placed strategically. Or, we found that there was no chair alarm at all. So when we investigated, we found that we actually did not have enough chair alarms to go around to every room if we needed it. So once we figured that out, then we ordered more chair alarms. Then, we trained staff and, um… in the strategic placing of the chair alarm, and to make sure we had chair alarms and batteries (laughs)-
Jen: Yes.
Gloria: Thanks to you, Jennifer, I have reminded staff that. And you know what? And that was the trend that we found for 2022. We resolved it. And to me, that was an easy fix.
Jen: Yes. Have you seen a reduction in your falls?
Gloria: Before we put all this in place, our average fall rate was 125 days seemed like the most we could get before there was a fall with or without injury. Mostly, thank goodness, our falls we haven’t had… just a few in the years past with injuries. But for 2022, and so far for 2023, we have had no falls with injuries. We have had falls, but right now, we are sitting at 214 days without a fall. And we have a promotion going on that if they can make it 365 days without a fall, that we have a big surprise for ’em. So everybody’s talking about it. And it’s a continuous project. And every day I round… That’s the biggest thing that I feel like has made a difference. I round every day and let all staff know where we’re at with the fall prevention. I put up postings how many days without a fall. And I just keep it in the conversation every day. And when they see me they say, “Oh, there’s the fall lady.” (laughs)
Jen: (laughs) That’s great. Sounds like you’ve had a lotta success for that, and good luck going forward.
Gloria: Thank you.
Jen: Yes.
Gloria: Thank you. Well, Jennifer, I would like to know, how did you decide to reduce falls?
Jen: So, we decided after, you know, reviewing our quarterly performance improvement studies, that we had opportunity our fall numbers were going not in the direction that we wanted them to. So we decided to go ahead and take action. Um, one of the first things we did was to develop a committee of staff that were dedicated and passionate about reducing falls. So part of that committee was that we engaged nursing management, frontline nurses, support staff, and physical therapy on reducing our falls.
Gloria: Well, what are some of the things that your committee did?
Jen: We had a great opportunity to participate in a presentation that was done by a national speaker who has a passion for the reduction of falls and reduction of falls with injury. And we were able to take some really valuable information and suggestions back to our organizations. And this is some of the things that we did. We changed our fall risk assessment, that was first and foremost, to the Johns Hopkins Fall Risk Assessment Tool, because we felt this gave us a lot more broadened perspective of our patients’ fall risk. We actually purchased the rights for the evaluation tool. And then we updated our fall risk action planning using a red, yellow, green scoring category based on their score on that fall risk tool. Um, and then we placed corresponding colored magnets on their door threshold so that passersby would know, those that were trained, if they’re red, they’re high-risk, they need to have two assists when they’re up. If they’re yellow, they’re moderate, they need one assist. And if they’re green, they can be up on their own. And of course, we educate all staff on that, including our non-clinical staff, so that, you know, if they’re walking by a patient room, they see a patient attempting to get out of bed, that they can immediately notify the nurse. Um, this training’s actually done at our new employee orientation and that includes staff such as maintenance, IT, and environmental services, administration, finance, because we are all responsible to keep our patients safe.
Gloria: Yes. And that’s what we’re trying to promote too because I don’t think a lotta people… they really thought it was just nursing staff that was responsible. And that’s what we’ve promoted too. And I feel like that has definitely made a difference in our fall reduction.
Jen: Yes.
Gloria: Were there other changes that you made?
Jen: So yes, we did assess our patient care environments for… like, patient rooms and such, for things that could lead to injury with a fall. So while we know we can’t prevent every fall, we can really reduce the risk of injury. And I like to just tell a little story about not preventing every fall. Um, in that we had a gentleman that was an inpatient, and he was in his lower 60s, and a strong, healthy man. And he was standing in his room one evening trying to find the baseball game on his remote-control TV and was not able to. So the nurse came in and she took the remote and she was trying to get it for him. And they were both looking at the TV as he preceded to step backwards to sit down while she found the channel. And he sat down and completely missed his chair.
Gloria: Oh, no. (laughs)
Jen: So there was a fall (laughs) in a man that really didn’t have a risk for fall. And fortunately, there was no injury. But in other things, you know, to prevent injuries, we did move, like, bedside stands that have sharp corners. We purchased some floor mats that we can put by patients’ beds that are at risk of getting out of bed, so if they fall there is less risk of injury. We purchased new bed and chair alarms that go under the patient without attaching to their gowns. And have purchased a few beds with built-in alarms. And again, we have reminded our staff to make sure that they’re checking those batteries on those chair alarms. We did have a dead battery one time that the alarm did not go off. And fortunately, we’d had no bad outcome from it, but it was a good learning experience, so…
Gloria: Well, Jennifer, I feel like if we tell everybody anything, it’s the battery.
Jen: Yes.
Gloria: Thank you for reminding me how important that is, ’cause you definitely helped me and I took it back to my staff and they’re like, “Oh my gosh, that’s a great idea.” Check the battery.
Jen: Great.
Gloria: Were there other things that you did from the environmental standpoint?
Jen: Yes, we did educate staff on making the patient room a little more user-friendly for the patient. So depending on what their need is, we can rearrange the room to ensure the- they have a clear path to their chair or to the bathroom. And then also, we educated on the use of gait belts and other equipment that are… could be needed for patients. And it is an expectation to have those things handy at all times.
Gloria: Well, what about footwear? Do you require anything in particular?
Jen: Oh, you know, that’s always a risk factor. If they bring their own slippers in, we wanna make sure they’re nonslip. But we did go about purchasing our own non-footwear. Co- course we had some previous to this. But we did an evaluation of some of the products that are out there to purchase and found that some actually tended to give a higher risk because they were sticky on the floor. We felt that would make a higher trip hazard. So we did find some that we liked, and that’s what we are using now.
Gloria: Wow, that’s great. How do you evaluate your falls and your program?
Jen: Well, every time there’s a fall, we have a fall audit that’s done. We always screen for the things that coulda been a factor in the fall, from… anything from the last rounding and bathroom break, to recent lab values. Las dose of meds that could trigger a risk, like pain meds or sleep meds just to name a few things. And then these audits help us look for trends and opportunities for improvement. And then, of course, from those, you know, we send out our education or make our process changes. We first implemented our changes on the med-surg floor, which is where we have all of our inpatients, our observation patients, and our swing bed patients, and have expanded that to the emergency department.
Gloria: That’s great. Have you noticed improvement in your fall rates?
Jen: Yes. We have really seen a decrease in both falls and falls with injury. And our patient numbers are, are low, but in the past four years, we’ve seen a greater than 50% reduction in falls and a greater than 75 percent reduction in falls with injury.
Gloria: Oh my gosh.
Jen: While we would like that number to be zero, we’re really happy with the progress that we’ve made.
Gloria: Yes. I know. And we both realize that it’s impossible to have 0% of falls.
Jen: Right.
Gloria: We would love for it, but, yes. So we’ve really enjoyed talking about fall prevention and hope you take back some great ideas to help reduce your fall risk because I got some great ideas from Jennifer, and I hope she got some great ideas from me.
Jen: I sure did. And we also appreciate the National Virtual Quality Improvement Mentor Program for allowing us to share performance improvement, so thank you.
Gloria: And remember, everyone can reduce fall risk! Thank you so much.
Jen: Thank you.