“I think it’s just all about relationships and making sure you involve everybody.”
March 2021
In this second leadership-focused session of Sharing PIE, executive, board, and clinical representatives from Sparrow Clinton Hospital in St. Johns, Michigan, share examples of how their board and senior leaders are engaged in helping drive quality outcomes.
Want to take Quality Time with you on the go? You can subscribe to the podcast version through your favorite streaming service.
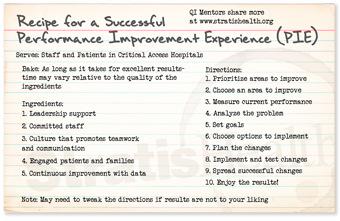
Insights from your QI Mentors
 Mariah Hesse, BSN, RN, CENP
Mariah Hesse, BSN, RN, CENP
Director of Patient Care Services
Sparrow Clinton Hospital
St. Johns, MI
Check out my favorite pie recipe below!
Second helping of PIE?
If you would like more information
from the national virtual Quality
Improvement Mentors on their
performance improvement
experience in critical access
hospitals, please submit this
short form.
| QI Mentor favorite featured pie recipe: Dutch Apple Pie |
 |
Transcript: How Board and Leadership Drive Quality Outcomes
Note: Quality Time: Sharing PIE is produced for the ear and designed to be heard. This transcript is intended to augment the recording.
Narrator: In this episode of Sharing PIE, leadership, board, and clinical representatives from Sparrow Clinton Hospital in St. Johns, Michigan, share examples of how board and senior leaders are engaged in helping drive quality outcomes.
Beth Daugherty: My name is Beth Daugherty. I’m president of Sparrow Clinton Hospital. Sparrow Clinton Hospital is a 25-bed critical access hospital, and quality is very important to us here at Sparrow. We believe that safety of our patients, our caregivers, and the quality of care that we provide every day is first and foremost as part of our strategic direction, looking to our future, and who we will be in the future, and how that fits in with our mission and values at Sparrow Clinton Hospital.
And the board is very engaged, but what makes the board so engaged, I think, is that our frontline caregivers provide a lot of the information to the board. And when the board hears it from the frontline caregivers, they realize it’s real.
Amy Palus: My name is Amy Palus, and I am the current board quality chair for Sparrow Clinton Hospital. I’ve been a part of the St. John’s Community for many, many years, working, raising a family. And I- I feel very engaged, um, because this hospital makes a big difference for our community, and I think as a mother, and as a community leader, I bring a different insight to the board.
Marcy Snyder: My name is Marcy Snyder. I’m a clinical nurse here at Sparrow Clinton. I worked in the Infusion Center and the Oncology Center for about five years. I’m the chair of the nursing quality education council, where bedside nurses get together every month and talk about quality and safety issues, education issues, and work directly with the management team, and also present at board meetings.
Mariah Hesse: And my name’s Mariah Hesse, director of patient care services and quality, and interim CNO at this time. And we are very lucky at Sparrow Clinton to have such an engaged board, and leadership, um, driving the way for quality and safety.
Beth Daugherty: We are one of three critical access hospitals in the health system. We are a primary employer in the community, but more than that, I think, we’re the heart of the community. We provide so much to this community that goes along with wellness and healthcare, and just being that heart and soul of a community. They know that they can come here regardless of what their needs are, and we try to accommodate that.
Narrator: The Sparrow Clinton group told us about the innovative approach to board rounding their quality committee uses to connect board and leadership to real-time improvement initiatives.
Amy Palus: We meet every other month, so the opposite month of a main board meeting, and that meeting is really focused on hearing from the different departments what is going on, what different structures they’ve put into place to put them at their different levels. They report back on employee engagement as well. Part of that board quality, we also started board rounding from, and every board member is e- is encouraged and the board rounding can be either… my very first one was watching an operation, to watch the different steps that each individual in the operating room has to go through.
Oher board rounding, um, recently completed was going through our second floor. So it was a tour where, we were shown, some of the improvements that have been made to that floor, also able to speak to different departments, and it just really lets the employees of Sparrow Clinton see that the- the board members are very interested in what is happening in the hospital.
Marcy Snyder: And as a- a direct caregiver nurse, this is Marcy, um, I’ve witnessed the board members coming around through the unit and asking questions, and touring, and- and just meeting us on a one-to-one basis asking if we have needs or any questions. I’ve presented at quite a few of the board meetings about projects, or initiatives that we’re starting, and they’ve always been very receptive and, you know, ask appropriate questions, and taking everything into consideration of what the direct caregivers need here at Sparrow Clinton.
Amy Palus: 04:58 I think it gives the board members, and the staff, the feeling of an open, honest, um, forum, like if they ever had any questions, I think, that we open that door for questions and a conversation to take place.
Mariah Hesse: Some will come already with questions in mind that they ask caregivers, for example, if you were the CEO for the day, what would be the first thing you would change? Another quick, good question is, do you feel free to speak up? What keeps you up at night? Any of these types of quality or safety, or do you have any safety concerns? And I think that is so great for caregivers to hear from the board.
Mariah Hesse: Also I think the caregivers can see the follow-through, some may say for patient safety, or for caregiver safety, or staff safety, they were complaining about some chairs in our lab department, and they complained, not complained, had that concern, voiced that concern-
Beth Daugherty: (laughs).
Amy Palus: (laughs).
Marcy Snyder: (laughs).
Mariah Hesse: … to the board members, (laughs, and lo and behold, the board members take it to the board meeting, on the- the target manager is made aware, and the lab got new chairs, and they thought, “Oh, wow, this is a great venue to be able to explain to the board different issues or concerns.
Every time after a board member rounds, they, we, they do a presentation at the next governing board meeting on exactly what they learned during rounding, the positives, the opportunities, the highlights, so it even takes it to that next step, which I think is very valuable
Mariah Hesse: I think another thing that’s really good to add is when the board members are rounding, they do it at different shifts. So we’ve had board members round in the evening. We’ve had them round, um, early morning. We’ve had them round in the middle of the day, and they all really try to rotate throughout different departments in the organization, even off-site at our rehab center.
Narrator: The Sparrow Clinton group went on to illustrate how important the patient voice is to quality improvement.
Beth Daugherty: The one thing that Amy mentioned that I think has also emphasized quality, that is very special for all of us is, we try to have a patient voice begin all of our quality meetings, and that patient voice oftentimes share with us what opportunities we have for improvement as well, and with that we try to tie that into the presentation that we’re doing that night. So if a nurse from the Infusion Center is doing a presentation, it may be an oncology patient, or an oncology patient’s family member who may be the patient voice to tell what occurred that had an impact on them, be it positive or negative, and then we talk about what we did differently, or what we will continue to do, to have that positive experience. So the patient voice is a great way to start each of our board meetings, and it’s always so welcome, and it puts a smile on all of our faces, and sets the tone for the whole meeting.
And a lot of the patients come to us with opportunities for improvement, (laughs)-
Marcy Snyder: And I’ll add onto that patient voice. It is a highlight of our meeting, whether it is negative or positive feedback, and a lot of times, you know, if there is that negative feedback, the patient that is- is getting the opportunity to speak in front of the board, speaks volumes to them. It shows that we care, we- we are listening and we want to do better.
Narrator: We wanted to hear from the Sparrow Clinton group about board commitment and participation, including how many members of the board are required to participate in their quality sub-committee.
Beth Daugherty: When you ask us how many board members are required, we all made a face-
Amy Palus: (laughs).
Marcy Snyder: (laughs).
Beth Daugherty: … because usually the whole board shows up-
Marcy Snyder: Yes.
Beth Daugherty: … so we’re not real sure.
Beth Daugherty: Part of our success with quality here is our commitment to resources, in order to have the board, the caregivers, everyone here at Sparrow Clinton engaged in quality, you have to make sure you have the resources available. And sometimes those resources mean having a nurse stay over for an extra four hours to work on a project. And during these times when resources are so tight and it still is critical to our mission and our values, and as the president of the hospital, you have to make those kinds of commitments to make sure that the staff know we’re committed to quality, the board knows we’re committed to quality, and we make sure that we’re looking at our resources from different perspectives to make sure that we can make it happen, to have a safe quality environment that is driven by our frontline caregivers.
Narrator: We asked the Sparrow Clinton group for an example of board members affecting change as part of their quality rounding.
Beth Daugherty: Our negative air pressure, the gauge on the door was reading different than what the gauge on the panel that is monitored by the air exchange company was saying. So we had a disconnect there. And so the caregivers in the ED were concerned about the patient’s safety, as well as their safety, for a negative pressure room.
So we had, the air handling people come in, for lack of better terms, um, that do that and have that expertise, and they went through the ED and made sure that all the gauges were appropriate, and we were getting appropriate reads, and that the negative pressure room in the ED was working appropriately
And with that, that brought to life that we had some opportunity for negative pressure rooms on the med-surg unit where, um, our med-surg area is an older area and it, our negative pressure room we did not know if the gauges were reading appropriately in there. And so one thing led to another, and we ended up having the whole negative pressure room redone on the, um, med-surg floor to meet current standards of air exchange for negative pressure.
And that was all supported through a board quality rounding that started in the ED with a question about negative pressure, and that cascaded throughout the whole organization, and to, t- in today’s environment with COVID, um, we just most recently put in some air scrubbers, and HEPA filters to provide more negative pressure rooms for patients that we care for that come in with the coronavirus or suspected coronavirus. So, that all cascaded from a board member rounding, and somebody asking a question.
Mariah Hesse: I think another thing that comes out of board rounding, another example is engagement, is caregiver engagement, and that does play a vital role with quality and safety. You know, you have to have an engaged workforce in order for it to reach the patients and the families in communities.
Marcy Snyder: The board members are very approachable and very kind and warm and, you know, make it clear to us that they’re just here to answer questions and, you know, find out if we need anything.
Narrator: We learned that at Sparrow Clinton, board rounding with staff is complemented by staff participating in board meetings.
Mariah Hesse: I think another key is to actually have frontline staff, direct caregivers come and present to the board and that builds another relationship between the board and the frontline caregivers that, you know, they are the qua- heart and quality and safety in our organization, and building that relationship and that comfort, I think is also key, and so rounding helps doing that.
Marcy Snyder: Just going back just a second, just for advice for other organizations, versus talking about us in particular, is maybe direct caregivers should be invited just to attend and not do anything as far as speaking at a board meeting a couple of times first- and then that might bring a little bit more comfort, you know, to instead of just go and present, you know, maybe just go and attend one and sit and listen, because that’s a lot more comfortable to just be a little fly on the wall and listen.
Mariah Hesse: Patient safety, quality as mentioned from others on this panel today, it’s more than just the patients. It’s the patients, it’s the families of the communities. It’s our staff, it’s our caregivers, it’s all of us working together in collaborative.
Beth Daugherty: I think it’s just all about relationships and making sure you involve everybody.
Narrator: Quality Time: Sharing PIE was produced by Stratis Health, with funding through Rural Quality Improvement Technical Assistance — a program supported by the Federal Office of Rural Health Policy — to help critical access hospitals across the country move from quality reporting to quality improvement. Want another serving of PIE? Or have a burning question about rural quality improvement? Visit the QI mentors web page.