“It takes the board, it takes the frontline staff, it takes quality, it takes administration, it takes physician engagement, it takes all of us to make a good team.”
February 2021
In this episode, quality, clinical, and board representatives from Horizon Health’s Paris Community Hospital in Paris, Illinois, discuss how successful board and leadership engagement drives quality outcomes.
Want to take Quality Time with you on the go? You can subscribe to the podcast version through your favorite streaming service.
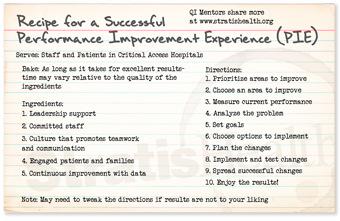
Insights from your QI Mentors
 Amy Arnett, MS, RN, CPHQ, CPPS
Amy Arnett, MS, RN, CPHQ, CPPS
Quality/Infection Prevention/Credentialing Manager
Paris Community Hospital
Paris, IL
Check out my favorite pie recipe below!
Second helping of PIE?
If you would like more information
from the national virtual Quality
Improvement Mentors on their
performance improvement
experience in critical access
hospitals, please submit this
short form.
| QI Mentor favorite featured pie recipe: Peanut Butter Pie |
 |
Transcript: Involving Board and Leadership to Drive Quality Outcomes
Note: Quality Time: Sharing PIE is produced for the ear and designed to be heard. This transcript is intended to augment the recording.
Narrator: In this episode of Sharing PIE, quality, clinical, and board representatives from Horizon Health’s Paris Community Hospital in Paris, Illinois, discuss how successful board and leadership engagement drives quality outcomes.
Amy Arnette: Hi, I’m Amy Arnette and I am the quality infection prevention, credentialing manager at Horizon Health in Paris, Illinois. We are along the Indiana border and are a 25-bed critical access hospital that has multiple rural health clinics associated with our organization, and our nearest, bigger facilities that we transfer to, or that patients travel to are 30 minutes or right around an hour from our area, and we have a large group of visiting specialist providers that come to do various services for our community and clinic patients. And we do a pretty good volume of both the urgent care, the outpatient and surgery volume in our facility.
Jamie Houlihan: Hi, I’m Jamie Houlihan and I am a member of the board here at Horizon Health, and I am a member of the quality subcommittee of the board.
Tiffany Turner: Hi, I’m Tiffany Turner. I’m the chief nursing officer and the vice president of patient care services.
Narrator: We asked our three representatives to start by sharing, from their perspectives, how their board and senior leaders are engaged in quality work.
Jamie: A few years ago, we were utilizing a consulting committee to help the board. And we decided at that point that it was not a cost-effective solution for us. We weren’t really getting the bang for the buck that we were looking for. And so at that point, the board as a whole decided to make a bigger investment, both personally, and as a group to kind of take the reins ourselves and make a commitment to owning the board more ourselves than kind of contracting that consulting piece out.
Jamie: So we’ve all become more engaged in terms of, you know, wanting to know how things are going and the results that we’re getting in terms of the pace of patient satisfaction and quality.
Tiffany: So the board actually took an active role in trying to be more engaged while still staying at a high level. They don’t typically get into operations, but they ask questions. They are also, of course, members of our community. So they have friends and family in the community. So they have a vested interest to understand what we’re doing at the facility and to try to drive safety and quality measures.
Tiffany: And so having some engagement with those, uh, board members from an administrative level, then we can drive processes down to the staff to try to engage the staff, try to make them understand what the board hears in the community, what their questions are. They want to know why we aren’t at a hundred percent on different measures. And so then that challenges us and challenges the staff to kind of drive those processes and change the way we, we take care of some things.
Amy: And another way that the board leadership, uh, support our quality initiatives over the last several years, we now keep a spreadsheet and we report from our internal hospital quality improvement committee. We report, uh, both data submission and tracking and attendance at our quality committee meetings. That goes to leadership in the board, And when the board asked the question, “Well, not all of the departments are participating, not everybody’s coming and submitting data. Why isn’t, why isn’t that happening?” And so from that, it drove things back the other direction with support from hospital administration. The board suggested that, uh, I, as a quality manager start asking a department manager to come to each quality board committee meeting and present on what they’re doing in their department.
Amy: And initially we had, you know, plenty of departments, but when it started getting down to the point that not every department’s participating, the quality board said, “Start asking those who aren’t submitting data, let them come to the quality board and explain to us why they’re not doing that or why they’re not finding it important.” So that gives you a lot more backing when you’re going to leadership and saying, “Oh, I’m looking for who’s going to come to the next quality board committee. Who’s going to volunteer? If somebody doesn’t volunteer, I’m going to start selecting from some of those who are not participating.” And that kind of changes the dynamics.
Tiffany: It holds everybody’s feet to the fire. And, you know, the rock stars are still rock stars, but the people who are lagging behind have been brought along.
Narrator: We wanted to find out how those departments being asked to present to the board changed their engagement or outlook on quality improvement
Amy Arnette: One of the things that’s come from that is, you know, it’s easy sometimes to think of quality improvement as another paperwork exercise, more data to collect. But when you actually go to show administration and the board what you’re doing, and you give feedback on, you know, thank you. They ask questions about the department and showing interest in what you’re doing. I think it makes them feel proud of their department and engages them in a different level.
Narrator: Next, we asked how frontline staff implementing them are aware that leadership supports those improvement projects.
Amy: One, one of the areas that, helps reinforce that is when we do, regulatory or survey rounds, mock survey rounds and departments. One of the questions we always ask the staff is what’s your PI project? Not only what’s your PI project, but how’s your data? Where, where are you guys rating on that right now? And how do you specifically impact that to help drive that message home? We also do, reminders about survey type things and questions that are asked. And, and it’s really an enlightening thing when you see a surveyor stop to ask a housekeeper, a question like that, and they look happy when somebody asks them a question and they can answer it. It, it truly, you can see that they are interested and that they take pride in things.
Jamie: We also have communication boards in the break room, that we put up some of that information. they have their PI projects posted. We also do, uh, most managers do a weekly email and they send those out on Friday afternoon. And it’s just a touch base, little bulleted points that talk about different things, such as PI projects. Don’t forget to reassess your medications. Don’t forget to document your start and stop times on IV medications. don’t forget to, you know, we’re watching handwashing, whatever it particularly is. We, we are constantly reminding people via email, visual cues, like I said, in the break room and then doing the mock surveys where they actually have to participate.
Tiffany: I round daily on all of the clinical areas. So instead of it being a surprise and you know, they only see me during survey time, they see me every day.. I try to stay late some days, I try to come in early some days, establishing a rapport with the frontline staff is, is a significant building process. And because I have a rapport with the majority of our clinical staff, I then can tax them, and I then can challenge them and try to hold them more accountable.
Narrator: We were curious if there was interaction between board and frontline staff
Amy: Typically when we’ve had, for instance, a board member as a patient, you know, that’s getting a different perspective from them. They, they sit on the board and they hear some of the reports and things, but when they’re on that other side of the experience, they sometimes give suggestions like, you know, “It would be helpful in the bathrooms to have toilet risers, and we should have those in all the bathrooms.” Just different perspectives and they feel very comfortable with offering that input.
Narrator: Amy, Jamie, and Tiffany went on to describe the types and consistency of the data board members receive
Amy: Every few meetings at the request of the quality board, we actually have gone out to these public reporting data websites to show the board what’s available on a public website about our facility and to show them how they can go there and they can see our hospital compared to others in the area.
Jamie: As I’ve spent my time on the board, we do get that, that data consistently and we have changed survey reporting, and that has been really helpful just in time, as we see the data and see the results, we become comfortable with the format and learn to be able to ask questions because we get comfortable seeing it.
Tiffany: So I think one of the things that I’ve been able to witness from sitting on this is when we first started out, our HCAHPS scores were quite low or just mediocre. And then over the course of time, like Jamie said, we changed to real-time information and we can, look at the real-time information on a dashboard and make changes, very rapidly versus waiting three months or, and getting that data, on a behind, the timeframe. So what that has allowed us to do is to change the direction of our HCAHPS scores.
Tiffany: We went from a mediocre score to fives across the board with our last report. Not only does the board see that, but then we’re able to translate to the frontline staff that they’re doing a very good job and that we can co- you know, we can give them the kudos that they deserve, for meeting all the metrics.
Narrator: We asked the representatives how much the board works in partnership with frontline staff to make implementing performance improvement initiatives happen.
Amy: One of the, uh, initiatives or measures we’ve been working on is sepsis most recently. And that’s brought about a lot of changes with the quality board saying, you know, “We’re not doing as good as we want to be here. If I’m the patient or my parent’s a patient, I want them to get the best care that they can.” And that has led to everything from changes in the physician or provider order set, education to staff, education to the providers, an interdisciplinary team that has met to including everyone from lab to the ED, to nursing, to administration, to just try to figure out how to get to the best way to not only to meet the measure but to make sure we’re providing that care the best way we can. Meeting the measures, the byproduct of providing that best care that we want to give.
Tiffany: It’s all a collaboration. We don’t do anything from a ‘me’ perspective or an ‘I’ perspective it’s all about a ‘we’. So, it takes the board, it takes the frontline staff, it takes quality, it takes administration, it takes physician engagement, it takes all of us to make a good team. And so with, you know, again, somebody might have a suggestion and then we build on it, or we, we implement it based on what, how they see that it would fit into their workflow. So it’s not just an end-all, you’re going to do this. Everybody has a piece in the project,
Narrator: We wanted to know how the representatives incorporate the voice of the patient to help inform their work with the board
Jamie: Every month, Tiffany brings an example to us, of someone who has had an experience that was really good, usually, (laughs), because we like to hear the good news –
Tiffany: They hear the bad, but they also want to hear the good. So, that’s one of the things, I bring a testimonial, uh, sometimes that is offered up via a staff member. Sometimes that is the patient who directly calls. Sometimes it’s a family member in the community that brings it. It just comes from multiple different sources. Again, the community is quite small, so we get those stories. I got one today about a patient who was having stomach issues and she had been to, very large facilities trying to get her stomach issues resolved.
Tiffany: And she said, she went, to one of our local providers and within a couple of days they had some answers. So not only were, is she very appreciative of the dedication that the provider gave her, but then the provider ordered, testing that was timely and appropriate. Uh, we were able to get her in with the general surgeon who was then very kind and took time with her, and then she was able to have surgery scheduled within a short timeframe and she’s home recovering now and feeling much better. But she said, you know, literally, it took a village to get us to where we are. And, because of everybody’s collaborative effort, she really felt like she got the best possible care and felt like she wasn’t a number, that she was truly a person that got the care that she needed.
Narrator: Quality Time: Sharing PIE was produced by Stratis Health, with funding through Rural Quality Improvement Technical Assistance — a program supported by the Federal Office of Rural Health Policy — to help critical access hospitals across the country move from quality reporting to quality improvement. Want another serving of PIE? Or have a burning question about rural quality improvement? Visit the QI mentors web page.