“Just because that patient has left our doors at the hospital doesn’t mean they’re not still our patient.”
August 2023
In this session of Quality Time: Sharing PIE, mentors Linda Webb from Pulaski Memorial Hospital in Winamac, Indiana, Stacey Karvoski from Wallowa Memorial Hospital in Enterprise, Oregon, and Tammy Sudtelgte from Floyd Valley Healthcare in Le Mars, Iowa share the varied approaches their teams have used to reduce avoidable hospital readmissions.
Resources from this episode
- Pulaski Memorial Hospital Heart Zones Tool
- Pulaski Memorial Patient Interview/Readmission Chart Review Tool
- Cynosure Health Readmissions Discovery Tool (used with permission)
Want to take Quality Time with you on the go? You can subscribe to the podcast version through your favorite streaming service.
 Linda Webb Linda WebbPulaski Memorial Hospital Winamac, IN |
 Stacey Karvoski Stacey KarvoskiWallowa Memorial Hospital Enterprise, OR |
 Tammy Sudtelgte Tammy SudtelgteFloyd Valley Healthcare Le Mars, IA |
Transcript: Fall Prevention Strategies
Note: Quality Time: Sharing PIE is produced for the ear and designed to be heard. This transcript is intended to augment the recording.
Narrator: In this session of Quality Time: Sharing PIE, mentors Linda Webb, from Pulaski Memorial Hospital in Winamac, Indiana, Stacey Karvoski, from Wallowa Memorial Hospital in Enterprise, Oregon, and Tammy Sudtelgte from Floyd Valley Healthcare in Le Mars, Iowa share the varied approaches their teams have used to reduce avoidable hospital readmissions.
Linda: My name is Linda Webb. I am the Chief Nursing Officer at Pulaski Memorial Hospital in Winamac, Indiana. We’re located in the northwest part of Indiana, about two hours south of Chicago and two hours north of Indianapolis. That kind of gives you [an idea of] where we’re located. We are a small rural critical access hospital with an average daily census of about seven. And our ER volumes are around 400 a month.
Stacey: I’m Stacey Karvoski. I’m the Quality Improvement Director and Risk Manager for Wallowa Memorial Hospital located in Enterprise, Oregon. We are a very small frontier critical access hospital located in northeast Oregon. We are four hours from Boise and about six hours from Portland. So, we’re in the northeast corner of Oregon. Our average daily census is about four, and our ER volumes are about 250 a month.
Tammy: Hi. My name’s Tammy Sudtelgte. I am the RN Quality Coordinator at Floyd Valley Healthcare. I’m also involved in patient experience and utilization review work here. Floyd Valley Healthcare is located in Le Mars, Iowa. We’re in the northwest part of Iowa. Actually, our community is known as being the ice cream capital of the world. Lots of ice cream produced here.
Host: So this podcast is about how your hospitals work to prevent readmissions. And readmissions are so complicated. And I know you each had different areas that you were focusing on. Tammy, if you would go first, and then Stacey and Linda. So, I’ll turn it over to you, Tammy.
Tammy: Our journey regarding readmissions actually began several years ago. I believe it was as far back as 2014, 2015. in reviewing the data from our Iowa State Hospital Association, we noticed that our facility was quite a bit higher than the state average for readmissions, and that tends to dent one’s pride a bit. Just like at most critical access hospitals, our patients are our neighbors, our friends, and our families. And we just knew that we wanted to do better for our community.
So intentions really were to reduce our readmissions, just more fully understanding our shortcomings and seek out opportunities for improvement. And then to do that by focusing on collaboration as we made efforts to improve. Our team here really gained momentum from hearing different presentations. We heard about community coalitions. We also participated in programs through our Avera Health system here and heard about initiatives related to care transitions. So those things were really key in launching our work. One key takeaway we chose to pursue was the community coalition concept. We oftentimes identified that there were just communication gaps in our patient handoffs and that collaboratively, we could do a better job to care for our shared patients with local care facilities.
So, in putting that work together and making that community coalition concept our own, we put together a countywide team that included clinical representatives from each care facility in our county and each assisted living, included our local primary care clinic, home health, public health agency. We had a lot of hospital representation, nursing, discharge planning, quality, social services.
The core group really was key in developing this coalition. Through the coalition, we were able to identify and address gaps in day-to-day communication processes, just little things that we would do on hand-off that made for lack of clarity or made for a lot of work on the receiving end of things, for instance, something as simple as a Tylenol order. We would dismiss people from the hospital with an order that said, “Tylenol, one to two every four to six hours as needed.”
And when a nursing facility would get that order, they oftentimes staff med aids, and those people aren’t able within the scope of their practice to make those decisions. So, the care facilities were each time, having to follow up with the physician and get a more specific order. When we realized that, we just (laughs) took care of that problem from the get-go and eliminated some of that re-work,
That group also developed a lot of standardized checklists for exchange of information, established a routine for post-discharge calls to the care facilities just to make sure that everything was very clearly communicated, and allowed us to continually work on the apps.
just also really gave us a nice opportunity to share educational topics. We talked about early recognition of sepsis, and that was key with those care facilities. Just in general, gave a better sense of trust and building a closer relationship. We were able to put a face with the name, made it a lot easier to reach out with questions ongoing. So really felt like a good program. And we do still continue to meet less frequently than we had, but a couple times a year, we’ll get together. Another initiative that we’ve really embraced with our readmissions reduction program is to do a resource navigation visit, and that’s a visit that’s free of charge to all of our discharged patients, whether it’s geriatric population, or OB population, pediatrics, anybody really.
And we’re able to do that free through a grant through our state public health department. Doing those visits really lets us ensure that our patients are set up for success. We can get in the home and see if they really understand their meds, if they actually obtained them, just kind of assess their knowledge of their treatment plan. We can look at environmental factors that might be an issue and confirm that there is an adequate caregiver situation. So, those visits have really been key in reducing readmissions, and sometimes it even leads to that they can qualify for an actual home health service, and that collaboration with our public health department has been very nice.
Linda: Tammy, great work on that collaboration. One of the nuggets for me that I’m really impressed with is those discharge calls back to the facility, and those hand-offs, and focusing on that hand-off communication, ’cause I feel that that’s an area that we can improve upon because we think, oh, they’re going to a long-term care facility. We’ve given their instructions. Now they’re taking over that care. But being that resource, doing those calls, you know, we do follow-up phone calls with our, you know, when patients are discharged home. But I really like that touching base with the facility to say, “Hey, do you have any questions?” I, I really appreciate you sharing that, and the work that you did collaboratively throughout your community is really impressive. Thanks for sharing.
Tammy: Thank you. It’s really been enjoyable to feel like we’re meeting the needs of our patients and our community partners.
Stacey: Our readmission journey began probably four or five years ago when we put together our readmission reduction group that involved behavioral health, DHS, all the clinics, providers, mental health providers, community connections, who does Meals on Wheels and Meals for Folks. And we started getting together to figure out how we could reduce readmissions. Our journey’s been a rocky one due to staff changes and position changes and who’s responsible for what.
But I think we’re finally in a good state now, and we’re stable. We’ve got everything figured out on who does what. But one thing that came up in our quality improvement area was our EMS is having a lot of frequent calls to the same houses. So, we kind of roped them in with our readmission reduction as well, and we tried to figure out how we can help, how readmission reduction can help reduce the number of EMS calls to the same locations, because what we found was that most of those calls that EMS is going on for lift assists, somebody fell out of their chair, and they just wanted somebody to come help them get up, they refused transport.
Those people were our multi-visit patients. They were the ones that would come in. When they were admitted, they always ended up being a readmission. So, we’re trying to work on helping to reduce the EMS call logging, but also helping to connect those patients with services and making sure that they have the services they need.
What we have done is we used the Unite Us platform. It’s a community-wide platform that we just started using last year. All of our clinics in our community have Unite Us. The hospital where I’m on Unite Us, our social worker’s on Unite Us, behavioral health is, community connections, the folks that take care of seniors, caregivers, they’re on that as well.
We try to figure out how can we use that platform for referrals. And it is for referrals. So, you can get on Unite Us and say, “Okay, this person has a transportation issue.” We can do a referral to community connections, and then community connections will contact that patient and see how they can help with the transportation issue.
So what we’ve done to help the EMS situation is, when EMS goes on a run with these multi-visit patients, if they see that their medications are awry, or they see that they need grabbers or they see they need something, physical therapy, they will have that patient sign a consent for social work to contact them and for us to be able to put in contact a primary care provider.
EMS was trying to contact primary care via texting, and that wasn’t working. Our social worker has access to the EMS records. So, she can get on there and see that that is a multi-visit patient, and she will then get on Unite Us platform and do a referral to primary care, or to whatever service they need.
She’ll do a referral for a nurse visit for a care coordinator visit. And so, then the care coordinator will know, okay, this patient is having, having trouble in certain areas. And they will connect with that patient. They will either go to the house or they will call them, and they’ll make sure that they have a visit with primary care.
And now, with Unite Us platform, EMS knows that that happened, and so we’re able to close the loop and know that, okay, that patient was seen, they’ve signed the release, and a referral was done to care coordination or transportation or some other service that the patient needs. And then by getting on Unite Us platform, we can see that that referral was done and what the outcome was. So that’s actually helped connect those patients with the services they need and to make sure that they’re connected, and everybody can see that the loop has been closed and the follow-up has been done.
We actually have seen a reduction in the number of calls going to those same households, we’re seeing the reductions with the use of that, and I think that’s helping to ease the burden of our EMS call logs for patients that really don’t need transport and help to connect those patients to the services they may need.
That’s where the Unite Us platform came from because they saw that there was a gap in how we can do referrals to other agencies because most of us are on, all of our clinics are on Epic.
So, we can do referrals in Epic, but there’s these outlying agencies that aren’t on Epic that can’t get the referral. So, Unite Us allows us to make those referrals to those other organizations that maybe aren’t on our same electronic health record.
Linda: Stacey, again that community involvement, focusing on what are those social determinants of health, whether that’s from that mental health team, that coalition that you’re working with, but pulling all the health care entities together to really make a difference for your community.
And as we all know, or we all struggle with, with EMS, with transfers throughout the nation, and being able to kind of get rid of some of their barriers, that’s great work. Thank you for sharing.
Tammy: Stacey, I just think that the involvement with the EMS is just so interesting. I know every community (laughs) has those calls where they just need a lift assist, and it just makes so much sense to look at that and know that those folks are having some needs that are potentially unaddressed and to get the right referrals made based on those frequent calls is wonderful.
Stacey: Yeah. EMS is, you know, they’re another set of eyes in the house, and since they are obviously medical, they’re looking at other things other than just helping that patient out of the chair or whatever they need. So, it’s nice having that other set of eyes in the household that can help care for that patient.
Tammy: Absolutely.
Linda: Our readmission story started back in 2017, 2019, sitting in a PI meeting, and Anthem scorecard results came out, and part of that Care Compare through CMS, and yeah, we didn’t look so good. The focus was on the heart failure readmissions at the time. And so, we started putting a team together in 2000, and and then a pandemic took precedence over all that work. Some of the things we wanted to focus on is making sure that our order sets were up to date. looking at our discharge instructions and making sure that we have relevant, up-to-date information. One of the things you’ve asked us about is what those measurements look like, and, and how do we keep track. And again, if we’re not measuring something, we don’t know that we need to improve that. So as Tammy indicated, none of us want to look good when our scores are bad, but it gives us an opportunity to really focus, really drill down, and really look at improvement, and being critical access, with our numbers being lower, sometimes those percentages are, are higher.
So, wanting to focus on that foundation, our order sets, our discharge instructions, and what that looks like. Pull the team together with all those. We always have that saying, if you’re not at the table, you’re on the menu type of thing. Not only getting nursing involved but also getting cardiopulmonary, respiratory involved. how do we connect our patients post-discharge to cardiac rehab? because heart failure is one of those approved diagnoses to help our patients.
Our rural health clinics from that transition of care piece, having them at the table was very helpful. Having pharmacy at the table.
So, to Tammy and Stacey’s point is making sure that you’ve got all that support. Ours focused more internally as opposed to maybe some of those transition of care, and I’ll touch on that a little bit. We have zone sheets. We’ve had them for years too, and they’re what we use for discharge instructions.
They’re color-coded, green, yellow, red. It’s education that the patient can slap up on their refrigerator and say, “Am I having these symptoms today? What should I do?” We also felt it was important from that patient family engagement that we share our current zone sheets with our patients and say, “Do these make sense? Are these helpful? Is this gonna be beneficial when you’re discharged?”
One time I heard a speaker say, “Nothing about me without me,” and sometimes we tend to make changes at the hospital, but we fail to include the most important person, which is our patient and family. Our patients did appreciate our zone sheets, had some little tweaking recommendations. And so, we made those. I know part of the success is having champions, having champions that own this work.
Whether that’s our clinical leader who has a great rapport with our providers and our staff. But also having a physician champion. So when we have our programs, and we roll those out, they’re that voice that goes in front of the medical staff and explains why we need to make these changes. So I think that leads to success in the program. And you’ve got that ownership and that responsibility. So that’s very helpful.
The other thing when we talk from the patient family perspective, we are part of the Indian Hospital Association, we are part of the HQIC, the Hospital Quality Improvement Collaborative, which is funded through CMS. And they’ve partnered with Cynosure, and Cynosure has some really neat tools and education opportunities. Readmission Discovery tool is one of those items that we use. We wanted to get, from a patient and family’s perspective, why they felt they had a readmission to the hospital. Were they unable to obtain or take their prescribed medications? Did they have any issues understanding the discharge instructions?
Were they able to get to an appointment? Were there any specific social determinants of health that prevented their success at home, and maybe it created that readmission, such as food insecurities, transportation issues, or housing? We’ve seen improvement with heart failure numbers, our readmissions for heart failure, but we feel that it’s important that we’re still looking at all readmissions. So when you focus on heart failure and seen improvement there, how do we spread that then to other readmissions, say for COPD or any general type of readmission?
So, I think that’s then an important part as well. Working with our rural health clinics and helping our patients make that transition from the hospital to the home and then making sure they’re having the appropriate appointments. So having representation from our rural health clinics has been very important. Our team, our nursing leadership team, they’ve gone around to each of our rural health clinics, our outlying clinics, and explained the program to them, explained the education we’re providing in the hospital so then they have those same consistent tools when those patients show up in their clinics.
So, the rural health clinic staff really appreciated that work and that collaboration with the hospital, that’s been very positive. Transition of care, we meet quarterly with our long-term care facilities, home health care, mental health, to explain, you know, what we’re working on, whether that’s sepsis or readmissions, and how we work together. I think Tammy and Stacey really have a great community collaboration.
We’re not there yet. But you guys have certainly given me some great ideas on how to move forward and how to focus on some different ideas from that community perspective. You know, as you go along, you find some barriers. There’s indicators for all of this through our performance improvement program. And we had found that with high-risk readmissions, we wanted those patients to be seen in the offices within 48 hours.
Sometimes the discharge physicians would say, “Ah, I’ll see them in a week.” and so, we were falling out on that. So, we created a nurse-driven protocol. If it’s a moderate risk for readmission, we were making sure that we were seeing those patients within three to five days after discharge. If it was a high-risk readmission, then we were wanting those patients to have an appointment within 48 hours. So that nurse-driven protocol really did help, making sure that those patients were getting to the providers in a timely fashion. I think that’s all I have. (laughs)
Stacey: I have a couple questions. I love the zone sheets you’ve created. We have one for CHF, but how do you engage staff to actually give those to patients? Because they are helpful information because they give them kind of the information they need at a glance on when they should seek help.
Linda Webb: We have a discharge folder. The zone sheets we had developed several years ago, and we have them for our top probably 20 diagnoses. And that’s part of the discharge education that goes into that folder. And we monitor education from a PI perspective to make sure that the information is being given. Now, with our electronic medical record, we can click on Lexicon discharge instructions were given.
So, we actually had to build that to say the zone sheets were given so the nurse can click on that so then there’s that documentation too. It’s part of the discharge flow sheet in our electronic medical record. The other thing, when Tammy talked about that follow-up call with the nursing home, sending the zone sheet with our patients go to the nursing home so it could be posted on their bulletin board in their room. So, when family members come, and they’re sitting and talking with grandma and she’s complaining about her feet getting tight, that part of it is to help educate family members as well, even when they go not just home but to a long-term care facility.
Tammy: Linda, I really like your readmission patient interview. I think that’s just really key to picking up on little issues that we might not have even recognized, but even better than that, to take that information, like you are, and use it more broadly to look for gaps where you can just solve those issues for other patients as well. That’s really great.
Linda: Yep. Thank you.
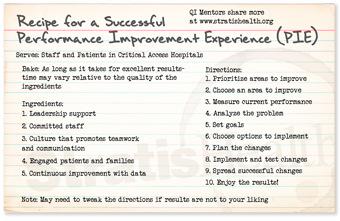
Host: So being quality improvement leaders and thinking about the ingredients in the recipe for successful performance improvement, which we call PIE, which one of the ingredients does each of your initiatives primarily focus on?
Tammy: My focus area as we look at the pie recipe touches on many of the ingredients but in particular, the culture that promotes teamwork and communication. As we work with that community collaborative, it takes a team. It’s all the different entities from the primary care clinic to a hospital and discharge planning, home health agencies, certainly the care facilities. And that we’re all moving in the same direction, and we all know the processes and workings of each other, that we make things line up and succeed is key. And then, of course, patient involvement as well, to be a partner in that.
Stacey: I would say one of the main things for us is committed staff. I think our staff are very committed to help these people succeed in their homes. And they’re willing to go that extra mile to go out to the home, make those referrals, go back if they need to. EMS has gone back. Cardiopulmonary has gone and helped patients in their home. We have a culture in our organization that really is about the patient and the patient’s why we’re here. And if we can keep them comfortable in their home and keep them from coming back to the hospital, that’s a win for us, a big win. I also think that engaging patients and families, because for patients to be willing to sign that consent form and have somebody call them and talk to them and come out to their home is a big deal, that they want to be engaged in their care and they want that help. So, I think without the patients being willing to let staff call them and do those referrals, it, it wouldn’t work.
Linda: From my perspective, when we look at the different elements for the success for any type of performance improvement, it’s the culture that promotes the teamwork, communication. And then once we have processes in place, it’s that accountability that everybody’s doing their role and that you’re measuring that as well. Making sure that when those patients come in, they can ask them about different things they should be watching for heart failure and making sure that they’re doing appropriate follow-ups. The one thing from that accountability or that teamwork is just because that patient has left our doors at the hospital doesn’t mean they’re not still our patient. They’re part of our community. And how do we communicate to one another to make sure that, as in Stacey’s words that those patients are successful. And I think, Tammy, you said it earlier this is our community. These are our friends, our family members. We see them at church. We see them in the grocery store. And we wanna make sure we’re doing the best care we can. And so that teamwork, communication, and holding each other accountable is very important.